Picture: Typical findings in hyperhidrosis of the armpits
What is hyperhidrosis?
Hyperhidrosis, also known as hyperhidrosis, consists of the word stems hyper = a lot and hydro = water. This refers to abnormally heavy sweating that exceeds normal levels.
Those affected experience a clear illness value due to restrictions in their social and professional environment.
In the following, we will focus on primary hyperhidrosis (see below for an explanation).
Facts and figures
- 3% of people suffer from hyperhidrosis.
- Of these, around 50% are affected by focal hyperhidrosis of the armpits.(1)
- In 30-60% of patients, it can be assumed that the disease is hereditary, as family members are also known to be affected.
- Primary hyperhidrosis mainly affects the armpits (in 73% of cases)(2)
What are the causes and forms of hyperhidrosis?
Often no cause for excessive sweating can be found. This is referred to as primary hyperhidrosis. In most cases, this occurs in certain areas of the body and is therefore called focal.
In the case of secondary hyperhidrosis, diseases in the field of internal medicine, neurology or endocrinology (hormonal disorders) are responsible for the condition.
The number of sweat glands is not increased, but their stimulation is increased. This occurs via the nervous system (sympathetic nervous system).
The following forms of this disease can be distinguished:
Primary form:
- Hyperhidrosis axillaris: excessive sweating in the armpits
- Hyperh. manuum: excessive sweating of the hands
- Hyperh. pedum: pathological sweaty feet
- Hyperh. faciei: on the face
Secondary form:
Secondary hyperhidrosis can be caused by the following diseases, among others ( 3):
- Medication and drugs: Alcohol, some blood-thinning medications, antidepressants, amphetamines, etc.
- Hormonal causes: hyperthyroidism, gout, menopause, obesity, diabetic neuropathy, hyperglycemia, acromegaly, pheochromocytoma, carcinoids
- Infections: Malaria, tuberculosis, infective endocarditis, HIV, brucellosis
- Cardiovascular / respiratory system: heart failure, heart attack, lung dysfunction
- Neurological causes: Parkinson’s disease, peripheral neuropathy, stroke, after spinal cord injuries
- Malignant diseases: Leukemia, lymphomas and various other tumors
What symptoms are typical for hyperhidrosis of the armpits?
Those affected by hyperhidrosis complain of abnormally profuse sweating, without apparent exertion and without adequate temperature stress.
Even in the winter months, unpleasant sweats can occur. Clothes are constantly soaked with sweat. In addition, the odor can be annoying.
Clothes have to be changed several times a day. The quality of life is greatly reduced. Sweating in hyperhidrosis often occurs suddenly and without warning.
There are no clear laboratory parameters for diagnosis. The patient history (anamnesis) is decisive. Typical symptoms are a family history and the onset of excessive sweating during or at the end of puberty or in adolescence.
There are tests to visualize hyperhidrosis:
- The iodine strength test detects sweat by coloration (violet) and is therefore of a qualitative nature.
- Gravimetry, on the other hand, can measure the amount of sweat (e.g. in mg/min). Here, filter paper is first weighed, then placed on the areas affected by hyperhidrosis for a certain period of time and then weighed again. The difference in weight now corresponds to the sweat production within the corresponding time unit.
Hyperhidrosis axillaris is a focal hyperhidrosis.
Hyperhidrosis axillaris is localized hyperhidrosis in the armpit area. Although sweat production is normal in other areas of the body, it is significantly increased in the armpits.
If internal causes have been ruled out, axillary hyperhidrosis can be treated well by removing the sweat glands surgically or conservatively using Btx.
How is hyperhidrosis treated?
With regard to the treatment of primary hyperhidrosis, a distinction can be made between surgical and conservative procedures. It makes sense to start with conservative treatment. If this is unsuccessful, you can consult our Yuveo team in Düsseldorf about surgery.
Treatment concept (4):
In the case of primary hyperhidrosis, we generally recommend starting with the application of so-called antiperspirants such as aluminum chloride (deodorants).
In the case of hyperhidrosis on the hands and feet, it makes sense to try iontophoresis (described below).
If these methods fail on the hands, the last option is an endoscopic thoracic sympathectomy (described below).
In the case of axillary hyperhidrosis, Btx treatment should be carried out after the local remedies. If this is unsuccessful or is not desired in the long term, lipocurettage or endoscopic thoracic sympathectomy can be performed.
What surgical options can be used to remove sweat glands?
The main surgical options for the treatment of focal hyperhidrosis are lipocurettage and sympathectomy:
Sweat gland removal by lipocurettage is the most commonly used method and combines sweat gland suction with curettage.
Simple sweat gland suction has been largely replaced by lipocurettage.
In bare curettage, suction is not used. The sweat gland tissue is scraped out with a curette (a sharp spoon) through one or two small incisions.
Sweat gland excision (according to Skoog)
… has also been largely replaced by lipocurettage and is now only reserved for extremely stubborn cases.
Here, the area of skin affected by axillary hyperhidrosis is completely or partially removed and then closed.
In the past, so-called flap plasty was used to cover defects, but this meant significantly more scars and a higher rate of infections and wound healing disorders than with sweat gland removal by lipocurettage.
However, the advantage of sweat gland excision is a very good success rate of 90%(4). Possible complications include wound infection, scarring, skin necrosis and skin discoloration.
Sympathectomy
is also known as sympathicolysis. This procedure can be performed either endoscopically (ETS = endoscopic transthoracic sympathectomy) or CT-guided through the skin (percutaneous CT-guided sympathicolysis).
In the first variant, an endoscope is inserted into the inside of the chest to block the nerves in the back section that regulate sweating of the hands, feet and armpits.
Possible complications include hemothorax (bleeding in the chest), pneumothorax (collapse of the lung), Horner’s syndrome, injury to the thoracic duct (main lymphatic vessel) and damage to the phrenic nerve (responsible for breathing, among other things)(6).
So-called compensatory hyperhidrosis can also occur in other areas, which can be just as impairing as the hyperhidrosis on the hands and feet.
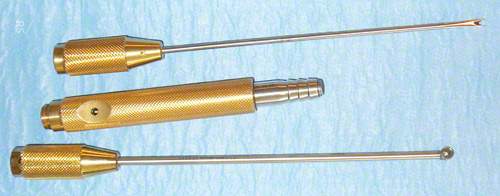
Picture: Instrument set for lipocurettage
What options are there for non-surgical treatment of hyperhidrosis?
There are various options for the conservative treatment of hyperhidrosis. The most important are aluminum chloride solution, iontophoresis and Btx injections.
Anticholinergics (menthanthelinium bromide, scopolamine and propantheline), antidepressants (amitryptiline and paroxetine), antihypertensives (beta-blockers, calcium channel antagonists (diltiazem)), alpha-antagonists (phentolamine) and alpha-2 agonists (clonidine) are discussed as possible medications for generalized, i.e. non-focal hyperhidrosis.
However, the study situation here is modest. These are often only individual case studies. In the AWMF guidelines(5), these medications for the treatment of hyperhidrosis are only considered with reservations.
Aluminum chloride
Aluminum chloride is the best-known treatment for hyperhidrosis without invasive surgery. The principle is to block the ducts of the sweat glands and thus block sweating.
It is a high-percentage solution that should be applied sparingly before going to bed. At the beginning (2-3 weeks) the aluminum chloride solution should be applied daily, after that it is sufficient to apply it about twice a week. Success is only noticeable after a few months.
The concentration of over-the-counter aluminum chloride solutions is less than 2% – pharmaceuticals, on the other hand, contain up to 25%.
Side effects: Due to irritation of the skin (redness, burning, stinging and itching), the treated areas should be treated with cream. The higher the concentration of the aluminum chloride solution and the more frequent the application, the more likely / stronger the skin irritation.
Discoloration of clothing! Therefore, wear appropriate clothing for this form of hyperhidrosis treatment.
Iontophoresis
Hyperhidrosis treatment using iontophoresis is another conservative approach.
The principle is also (similar to the aluminum chloride solution) to block the sweat gland ducts.
This is achieved by direct current flow during the application of baths. This treatment is well suited for hyperhidrosis on the feet and hands. The treatment should be carried out approx. 3 times a week at the beginning, later once a week.
Approximately 80% of patients with focal hyperhidrosis of the hands and feet respond to this therapy. The combination with glycopyrrolate (not yet approved: off label) in water is particularly promising(7).
However, this treatment can also cause irritation of the skin with redness, burning and blistering.
Btx treatment
It is a less complex form of hyperhidrosis treatment with few complications, which is expensive in the long term and limited in time.
Large quantities of the neurotoxin Bttx have to be injected into the affected areas, which chemically blocks the formation of sweat (release of acetylcholine is inhibited).
Unfortunately, the effect only lasts for 3-6 months, so that the treatment has to be repeated afterwards.
When treating hyperhidrosis of the feet and hands, symptoms of paralysis of the small muscles of the hands and feet may occur.
Literature:
1, US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. – Strutton DR, Kowalski JW, Glaser DA, Stang PE. – J Am Acad Dermatol. 2004 Aug;51(2):241-8.
2, An epidemiological study of hyperhidrosis. – Dermatol Surg. 2007 Jan;33(1 Spec No.):S69-75. – Lear W, Kessler E, Solish N, Glaser DA.
3, Sweaty, smelly hands and feet. – Scarff CE. – Aust Fam Physician. 2009 Sep;38(9):666-9.
5, AWMF: Guidelines of the German Dermatological Society (DDG) – Definition and therapy of primary hyperhidrosis – No. 013/059 – Creation date 02/2007
6, Transthoracic endoscopic sympathectomy in the treatment of palmar hyperhidrosis-with emphasis on perioperative management(1,360 case analyses). – Lin TS, Fang HY. – Surg Neurol. 1999 Nov;52(5):453-7.
7, Iontophoresis with glycopyrrolate for the treatment of palmoplantar hyperhidrosis – Dolianitis C, Scarff CE, Kelly J, Sinclair R. – Australas J Dermatol. 2004 Nov;45(4):208-12.